Everybody Hates Paperwork
Intake reports can be overwhelming and interrogatory. You are asking someone to give you as much details as possible about the most personal parts of their life. The goal of an intake form is to gain as much information about your client as possible before the initial interview. This way, you can begin to build rapport with your client during your first meeting instead of interrogating them about sometimes irrelevant details about their past relationships and work experience. Some ways to make intake forms more approachable is by including your therapeutic approach and goals at the beginning of your form. That way the client can feel a connection and motivation for filling out yet another monotonous stack of paperwork. Another important note is that traditional intake forms operate in the binary including limited options for self-reported identities. Offering “fill in the blank” options can be more welcoming to clients who do not fall into traditional binary categories like cisgender, heterosexual, monocultural individuals.
Covering the Basics
Basics include client’s name, age, date of birth, date of intake, intake interviewer’s name, and date of the report.
When creating your own intake form, Sommers-Flanagan & Sommers-Flanagan offer an outline for an Intake Report:
- Identifying Information and Reason for Referral
- Client name
- Age
- Sex
- Racial/Ethnic information
- Marital status
- Referral source (and telephone number, when possible)
- Reason for referral (why has the client been sent to you for a consultation/intake session?)
- Presenting complaint (use a quote from the client to describe the complaint)
- Behavioral Observations (and Mental Status Examination)
- Appearance upon presentation (including comments about hygiene, eye contact, body posture, and facial expression)
- Quality and quantity of speech and responsivity to questioning
- Client description of mood (use a quote in the report when appropriate)
- Primary thought content (including presence or absence of suicide ideation)
- Level of cooperation with the interview
- Estimate of adequacy of the data obtained
- History of the Present Problem (or Illness)
- Include one paragraph describing the client’s presenting problems and associated current stressors.
- Include one or two paragraphs outlining when the problem initially began and the course or development of symptoms.
- Repeat, as needed, paragraph-long descriptions of additional current problems identified during the intake interview (client problems are usually organized using diagnostic— DSM —groupings, however, suicide ideation, homicide ideation, relationship problems, etc., may be listed).
- Follow, as appropriate, with relevant negative or rule-out statements (e.g., with a clinically depressed client, it’s important to rule out mania: “The client denied any history of manic episodes.”).
- Past Treatment (Psychiatric) History and Family Treatment (Psychiatric) History
- Include a description of previous clinical problems or episodes not included in the previous section (e.g., if the client is presenting with a problem of clinical anxiety, but also has a history of treatment for an eating disorder, the eating disorder should be noted here).
- Description of previous treatment received, including hospitalization, medications, psychotherapy or counseling, case management, and so on.
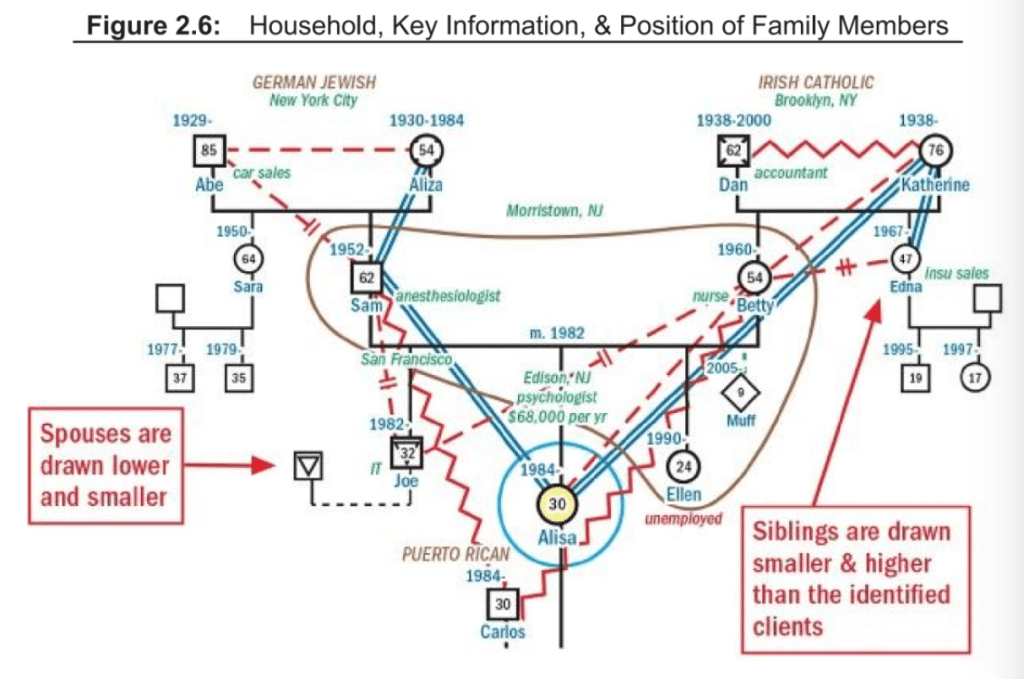
- Include a description of all psychiatric and substance abuse disorders found in all blood relatives (i.e., at least parents, siblings, grandparents, and children, but also possibly aunts, uncles, and cousins).
- Also include a list of any significant major medical disorders in blood relatives (e.g., cancer, diabetes, seizure disorders, thyroid disease).
- Relevant Medical History
- List and briefly describe past hospitalizations and major medical illnesses (e.g., asthma, HIV positive, hypertension).
- Include a description of the client’s current health status (it’s good to use a client quote or physician quote here).
- Current medications and dosages.
- Primary care physician (and/or specialty physician) and telephone numbers.
- Developmental History (This section is optional and is most appropriate for inclusion in child/adolescent cases.)
- Social and Family History
- Early memories/experiences (including, when appropriate, descriptions of parents and possible abuse or childhood trauma)
- Educational history
- Employment history
- Military history
- Romantic relationship history
- Sexual history
- Aggression/Violence history
- Alcohol/Drug history (if not previously covered as a primary problem area)
- Legal history
- Recreational history
- Spiritual/Religious history
- Current Situation and Functioning
- A description of typical daily activities
- Self-perceived strengths and weaknesses
- Ability to complete normal activities of daily living
- Diagnostic Impressions (This section should include a discussion of diagnostic issues or a listing of assigned diagnoses.)
- Brief discussion of diagnostic issues
- Diagnostic code and label from ICD-10 or DSM-5
- Case Formulation and Treatment Plan
- Case Conceptualization
- Include a paragraph description of how you conceptualize the case. This description will provide a foundation for how you will work with this person. For example, a behaviorist will emphasize reinforcement contingencies that have influenced the client’s development of symptoms and that will likely aid in alleviation of client symptoms. Alternatively, a psychoanalytically oriented therapist will emphasize personality dynamics and historically significant and repeating relationship conflicts.
- Treatment options
- Include a paragraph description (or list) of recommended treatment approaches.
- Case Conceptualization
While not all of this information may appear relevant to the client’s current presenting problem, it is important to learn the client’s context.
Intake Form Examples
A simpler version of the exhaustive list above can be found in Positive Psychology’s example intake form.
Another example from Positive Psychology is their intake form adapted for couples.
California Association for Marriage and Family Therapy offers a longer, more exhaustive intake form.
Ways to Accommodate Clients
Some ways you can accommodate clients with your intake process is ensuring they have access to the document. It is important for counselors to check with clients to see if they struggle with internet access or reading so accommodations can be made. Filling out the intake paperwork in person with your client can build rapport and create a stronger relationship with your client by personalizing a typically impersonal part of therapy.
Another way you can accommodate clients is by offering options in the intake paperwork that go beyond the binary. Most forms offer limited, binary options for gender, sexuality, and even culture. By offering a “fill in the blank” option for questions about identity, clients can feel free to include any identifier that feels right for them, not just the limited options available on the paperwork.
Overall, clients want to know that you are capable of understanding them and handling all their needs that may come up during counseling. Starting off on the right foot with intake paperwork is a crucial part of showing clients you are a competent and capable counselor.
Resources
Sommers-Flanagan, J., & Sommers-Flanagan, R. (2015). Clinical interviewing. John Wiley & Sons, Incorporated.
Sutton, J. (2022, November 10). 20 Useful counseling forms & templates for your practice. PositivePsychology.com. https://positivepsychology.com/counseling-forms-templates/
Montgomery, JD. (2017). How well do you know your new patient? The Therapist.





Leave a reply to Initial Meeting – Rookie Cancel reply